Category: Preemie
-

Preemie 101
With Olivia’s early arrival, we were welcomed into a brand new exclusive club: the world of preemies. We didn’t ask for this entrance pass and I wouldn’t wish our experience on my worst enemy. There were endless hours of waiting, grieving, worrying, and coordinating arrangements. As a mama-to-be, I had heard countless stories of women…
-
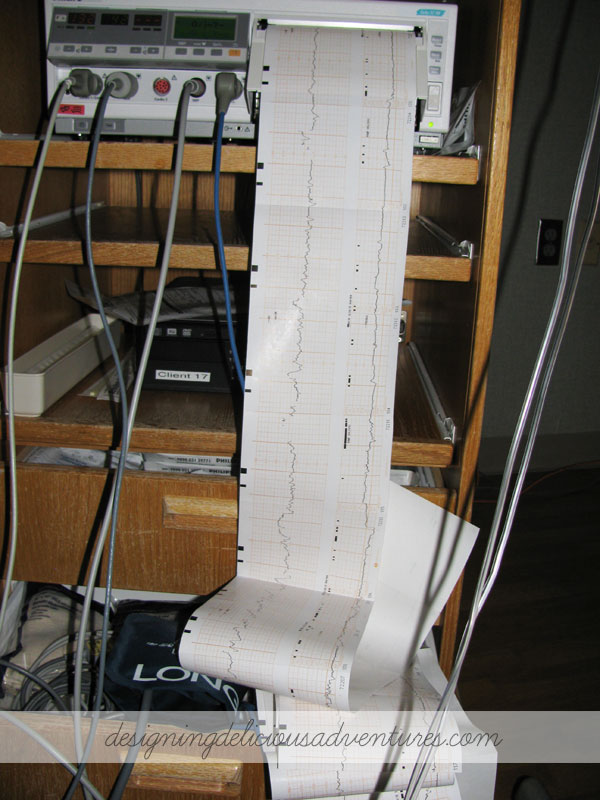
Olivia’s Birth Story: Part 2
This post is a follow-up to Olivia’s Birth Story: Part 1. After arriving at the hospital and facing the reality that we were going to meet our baby almost 7 weeks early, here is how our story unfolded: The doctor checked me at 1:30am and reported that I was already at 3cm, -2 station, and…
-
Olivia’s Birth Story: Part 1
I wasn’t sure how much of this story I was actually going to share on such a public forum. Why divulge the intimate details of such a meaningful and life changing moment? Reason #1: One of the lines in this post resonated with me. I could completely relate to Molly Mahar’s desire as a first…
-

The Day Time Stood Still
You might have noticed a bit of a time gap from my last post… our lives have been utterly transformed by one precious event: the birth of our sweet baby girl. Olivia Rose arrived on December 28, 2013 at 5:51 in the evening…. almost 7 weeks premature. I am not the same person I was…